Background
Pericardial fluid is a physiological fluid that is approximately 15-50 ml between the visceral and parietal pericardium of the heart in familiar situations. The liquid provides lubricity that facilitates heart movements, and together with the pericardium, it creates a barrier that protects the heart from external factors [1]. Pericardial effusion develops in cases where the production of pericardial fluid is increased, or its drainage is impaired. Depending on the elasticity of the pericardium, the increase in the fluid can be compensated to some extent. If fluid increases too quickly, it cannot be balanced with elasticity, and tamponade develops. If the increase in pericardial fluid is slow, large pericardial effusion may occur without the development of tamponade [2]. To the best of our knowledge, we presented the largest and most recurrent massive pericardial effusion case without tamponade.
Case Presentation
A 56-year-old man was admitted to the emergency department (ED) with a complaint of shortness of breath. The patient, who had no history of trauma or recent infection, had blood pressure (BP) of 187/140 mmHg, pulse rate of 81 bpm, respiratory rate of 20 breaths/minute, a temperature of 36°C, and SpO2 of 100% at the time of admission. He had heart failure and hypertension. Therefore, he used perindopril, amlodipine, and furosemide. A low voltage sinus rhythm of 80 bpm was detected in the electrocardiogram. Complete blood count, renal and liver function tests, electrolyte level tests, and cardiac troponin tests revealed no pathology. pH:7.17, pCO2: 91.5 mmHg, and HCO3: 24 mg/dl were detected. Chest X-ray showed cardiomegaly, which caused the image of a large heart almost filling the thorax (Figure 1). Thorax-computed tomography showed a large pericardial effusion reaching 16 cm at its widest point (Figure 2).
He was consulted with cardiology for pericardiocentesis and hospitalization. On Doppler echocardiography, 16 cm wide pericardial effusion was detected, but no signs of collapse or tamponade were observed. Cardiology recommended coronary intensive care unit (CICU) admission, but the patient was followed up in the ED until an available hospital bed was provided. We were informed that emergency pericardiocentesis would be planned if the patient developed hypotension during this period. Bi-level positive air pressure (BPAP) was planned due to hypercarbia, and the patient was connected to the ventilator device in BPAP mode with an appropriate mask. Since we expected that a hypotensive attack might develop when BPAP was applied, we prepared for emergency pericardiocentesis beforehand. After starting BPAP, the patient’s BP values decreased rapidly, and tachycardia was observed (BP: 102/85 mm Hg, heart rate: 133/minute). The patient’s hypotensive state was reported to the on-call cardiologist, and emergency pericardiocentesis was performed. A total of 6,000 ml of fluid was drained from the patient’s pericardiocentesis catheter.
Pericardiocentesis fluid was yellow. The fluid sample was sent to the laboratory. Lactate dehydrogenase and total protein values were asked to be analyzed from both pericardiocentesis fluid and blood samples. According to Light’s criteria, pericardial fluid was in transuda form. There was no colonization in the pericardial fluid culture. Bacteria were not seen in the Ehrlich-Ziehl-Neelsen (EZN) staining, and there was no colonization in the mycobacterial culture. In the microscopic examination, 20 leukocytes/mm3 were detected. The adenosine deaminase (ADA) test in the fluid was negative. The patient’s thyroid function test was normal. He received intermittent BPAP therapy due to hypercarbia during his CICU stay. He was discharged on the fourth day with the recommendation of antibiotic therapy and colchicine treatment after the fluid flow from the catheter was stopped. One week after discharge, 2.4 cm of pericardial fluid was detected. Drug allergy was considered in the patient with allergic skin lesions, and colchicine was discontinued. Ibuprofen was started. There was no increase in the pericardial fluid of the patient who came to the control after 1 month.
In his detailed anamnesis, it was learned that pericardiocentesis was performed twice, in 2013 and 2017. These admissions were briefly as follows: Complaints of dyspnea, pericardial effusion of 12 and 14 cm, respectively, 4,500 ml of pericardial fluid removal in both visits and no significant result in the examinations. He had a 3 cm pericardial effusion 2 weeks after his 2017 discharge. No echocardiographic records were available until the last admission.
Discussion
Massive pericardial effusion may not always present with signs of tamponade. Diagnosis can be made quickly with echocardiography, but it is more challenging to determine the etiology. Pericardial effusions may develop due to trauma, inflammation, malignancy, connective tissue diseases, infection, and endocrinological disorders [3]. The most common cause of pericardial effusion of inflammatory origin is idiopathic pericarditis. It usually develops after viral infections. Although a definitive diagnosis of viral pericarditis requires cytological and immunohistochemical examination of pericardial sampling, it is not applicable in clinical practice. Viral serologies are also not routinely recommended. The diagnosis of idiopathic pericardial effusion is made by excluding other diagnoses [3,4].
In immunosuppressed patients or if the history suggests bacterial or fungal infection, the culture of the pericardial fluid is necessary to guide treatment. Pericardial effusions caused by bacterial or fungal infections are typically exudative and may be purulent in severe cases. Often, these patients may show a more aggressive course and present with pericardial tamponade. Tuberculosis is the most common cause of pericardial effusion in developing countries and has a 17%-40% mortality rate within 6 months of diagnosis [4]. In patients with suspected tuberculous pericarditis, investigations should be conducted for active tuberculosis in other body parts. Pericardial fluid should be cultured. Polymerase-chain-reaction examination also helps in diagnosis. A positive ADA test from pericardial fluid is significant for tuberculosis-induced effusion [4,5].
Pericardial effusion may also be seen in malignant diseases such as lung, mesothelioma, breast, and lymphomas. Even pericardial effusion may occur as the first sign of the disease. In effusions due to malignancy, malignant cells will be seen in pericardial cytology [6].
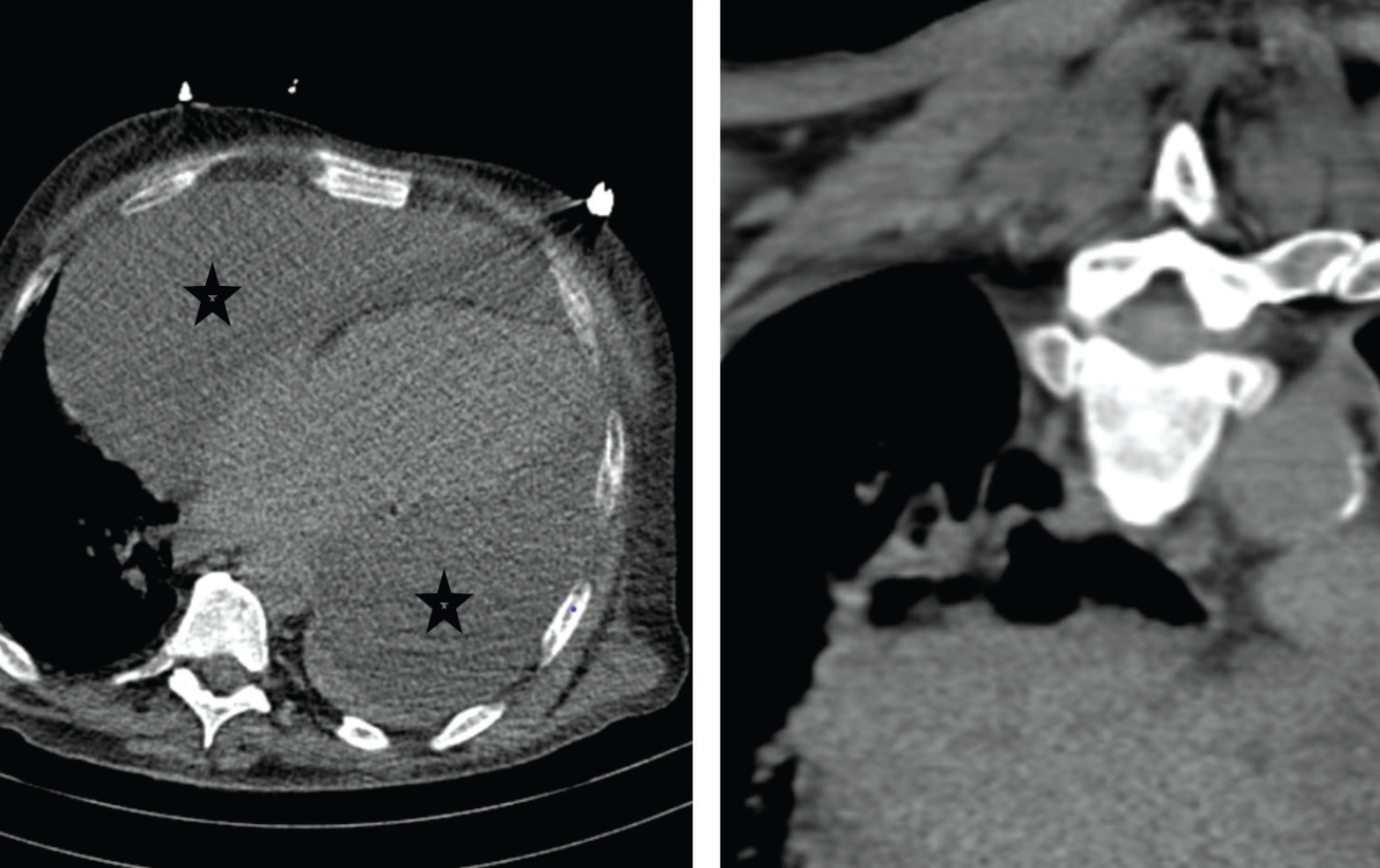
Large pericardial effusion reaching 16 cm at its widest point at CT scan. sign shows effusion sites.
Myocardial injury also causes pericardial effusion. After myocardial infarction, effusion may develop because the necrosis extends to the pericardium [7]. In our case, no clinical and imaging findings or laboratory results suggested acute coronary syndrome.
Uremia is a metabolic condition that can cause pericardial effusion. Pericardial effusion due to uremia is hemorrhagic; sticky fibrous exudates are seen in the pericardium. Another rare metabolic disorder that can cause pericardial effusion is hypothyroidism. Pericardial effusion may also develop in cases of severe protein deficiency due to malnutrition [1]. In our case, the patient had no malnutrition.
Patients with pericardial effusion are primarily asymptomatic. The rate of development of the effusion and the amount of collected fluid play a decisive role in the formation of the tamponade clinic. Pericardial tamponade develops in cases where 200-300 ml of fluid collects in the pericardial cavity within minutes, such as pericardial injuries. In cases where the pericardial fluid increases slowly, more than 1 l of fluid can accumulate without developing tamponade or any symptoms [8].
The amount of pericardial effusion can be evaluated with echocardiography. The pericardial cavity is less than 10 mm in pericardial effusions is considered negligible. In this case, the accumulated liquid will be <100 ml. If the pericardial cavity is between 10 and 20 mm, this is a medium-sized pericardial effusion, where the accrued fluid will be between 100 and 500 ml. The pericardial cavity is measured as >20 mm in large pericardial effusions, and the accumulated fluid is over 500 ml [9]. When the reported cases of large pericardial effusion were analyzed [10-13], it was seen that our case was the largest case of pericardial effusion without tamponade.
In patients followed up for pericardial effusion, mechanical ventilation may worsen the patient’s clinical condition, and there may be sudden decreases in BP values. The increase in intrathoracic pressure due to mechanical ventilation worsens venous return, leading to collapse due to further reduction of the limited cardiac expansion capacity [14]. Our patient was treated with BPAP due to hypercarbia respiratory failure during the ED follow-up, but his general condition deteriorated within minutes, and he became tachycardic and mildly hypotensive. Hypotension is a late finding and is often not seen until the pre-arrest stage due to natural compensatory mechanisms such as sympathetic tone and catecholamine response [2]. Therefore, the perception of hypotension as an indication of emergency pericardiocentesis should be changed. The amount to be drained is decided according to echocardiography and clinical follow-up in the literature, but, unfortunately, we could not find a precise amount for the pericardiocentesis threshold.
Small effusions can be followed without intervention. Fluid drainage can also be achieved in patients with large pericardial effusions without tamponade, but attention should be paid to pericardial decompression syndrome (PDS) [2,15]. When the pericardial fluid is drained rapidly, the patient’s clinic also improves rapidly, but after a while, PDS may develop with rebound dyspnea and pulmonary edema findings. Draining the fluid enough to regress the symptoms the first time is recommended. Afterward, it is recommended to discharge a maximum of 1 l at each intervention. It can be removed from the catheter placed in the pericardial cavity when it falls below 30-50 ml daily [15].
Conclusion
Even if the chronic pericardial effusion reaches enormous dimensions, it may not lead to cardiac tamponade due to the elasticity of the pericardial sac. Mechanical ventilation in patients with pericardial effusion can rapidly worsen the patient’s clinic. Pericardiocentesis should be performed first in patients who need mechanical ventilation.


