Background
Winged scapula (WS) is a deformity that occurs as a result of the dislocation of the medial edge of the scapula from the chest wall, resulting in pain, functional impairment, and cosmetic problems, and it is the most common scapulothoracic disorder [1,2].
Primary causes include neurological damage and bone and periscapular soft tissue pathologies, while glenohumeral and subacromial pathologies can be counted as secondary causes [3]. Also, WS may develop as a result of weakness of the serratus anterior, trapezius, and rhomboid major and minor muscles, which stabilize the scapula on the thoracic wall [4]. The position of the WS varies according to the affected nerve and subsequently weakened muscle. The most common cause of WS is a long thoracic nerve lesion, and the paralysis of the serra- tus anterior muscle occurs with this type of nerve lesion. Then, in the order of frequency of the etiology of WS, there is trapezius muscle paralysis, which develops as a result of a spinal accessory nerve (SAN) lesion. Rhomboid major and minor muscle paralysis, which may develop as a result of a dorsal scapular nerve (DSN) lesion, are more rare causes [2,5].
Case Presentation
A 39-year-old female patient attended our physical medicine and rehabilitation polyclinic with back, shoulder, and arm pain. The patient had undergone space-occupying lesion excision from the posterolateral neck region 3 years ago. The patient was told that the pathology result was good and no additional treatment was required.
Since then, she has had weakness and pain in her upper back, left shoulder, and arm. The patient complained that the pain started at the medial border of the scapula and radiated to the lateral part of the arm and forearm. The patient stated that she had difficulty in elevating her left arm. In this period, cervical MRI, shoulder MRI, and electromyography (EMG) examinations were carried out in the patient, whose pain complaints in her upper back, left shoulder, and arm and difficulty in elevating her left arm were started 3 years ago. The patient was diagnosed with cervical disk herniation, muscle pain, shoulder joint pain, and a SAN lesion. Pharmacological and exercise treatments were applied. In the EMG evaluation carried out at the outside the center 1 month ago, the patient was diagnosed with a SAN lesion. The patient was offered physical therapy. In the examination of the patient who attended our clinic for physical therapy, left-sided severe trapezius muscle atrophy, dropped shoulder, and mild scapular winging at rest were seen. With active arm abduction and flexion, winging in the left scapula became evident, and the upper and lower angles of the left scapula were displaced more laterally than the right side. However, the inferior angle of the left scapula was displaced more laterally than its superior angle. Cervical ranges of motion (ROMs) and passive shoulder ROMs were within normal limits. Active shoulder flexion and abduction were present in the range of 0-90°. Physical examination showed grade 3−/5 strength of left shoulder flexion and abduction, grade 4−/5 strength of left shoulder internal rotation, grade 4+/5 strength of left shoulder adduction, and other muscle strengths were 5/5. Deep tendon reflexes were normoactive, and pathological reflexes were negative. The provocative maneuvers used to diagnose thoracic outlet syndrome were negative. There was no abnormality in the hemogram and biochemistry tests. Shoulder MRI was reported as normal, but on careful re-evaluation, left-sided atrophy and increased signal intensity were seen in the trapezius muscle (Figure 1). Cervical MRI was reported as bulging at the C4-C5 and C5-C6 levels. The left shoulder and periscapular muscles were evaluated by ultrasonography (US). Meanwhile, it was observed that the thickness of the left trapezius muscle and the underlying left rhomboid muscle were lesser than the right side (Figure 2). US evaluation showed an increase in echodensity on the left side in the rhomboid major muscle and especially the trapezius muscles (Figure 2). Both sides of sternocleidomastoid (SCM) muscle thickness were measured as similar to each other with US (Figure 3). The point corresponding to the middle of the imaginary line extending between the origin (middle part of the clavicle) and the insertion (mastoid process of the temporal bone) of the SCM muscle was accepted as the reference point for the SCM muscle thickness measurement, and the measurement was made in the transverse plane. Firstly, for the measurement of rhomboid major and trapezius muscle thickness, the midpoint of the imaginary line extending between the inferior angle of the scapula and root of the spine of the scapula was marked, then a second point was marked as a reference point, which is 1 cm medial to the medial border of the scapula and 90° perpendicular to the first point. Since atrophy was detected in the left rhomboid major muscle, EMG examination was repeated. The EMG examination reported normal median and ulnar nerve sensory and motor conduction bilaterally. Long-term motor unit potentials with reduced pattern were detected in the left trapezius, levator scapula, and rhomboid major and minor muscles in needle EMG. Complex repetitive discharge activity was also observed in these muscles. The bioelectrical activities of the left deltoid, SCM, serratus anterior, teres major, teres minor, supraspinatus, and infraspinatus muscles were normal. As a result, these findings are consistent with chronic axonal degeneration in the segment of the left accessory nerve after innervating the SCM muscle and in the left DSN. Nonsteroidal anti-inflammatory drug was prescribed to the patient. The patient was referred to a rehabilitation program. A home exercise program has been organized for the post-treatment period. At the control visit 5 months after the treatment, the patient’s left shoulder active joint ROMs was within normal limits, while shoulder flexion and abduction muscle strength was 3+/5.
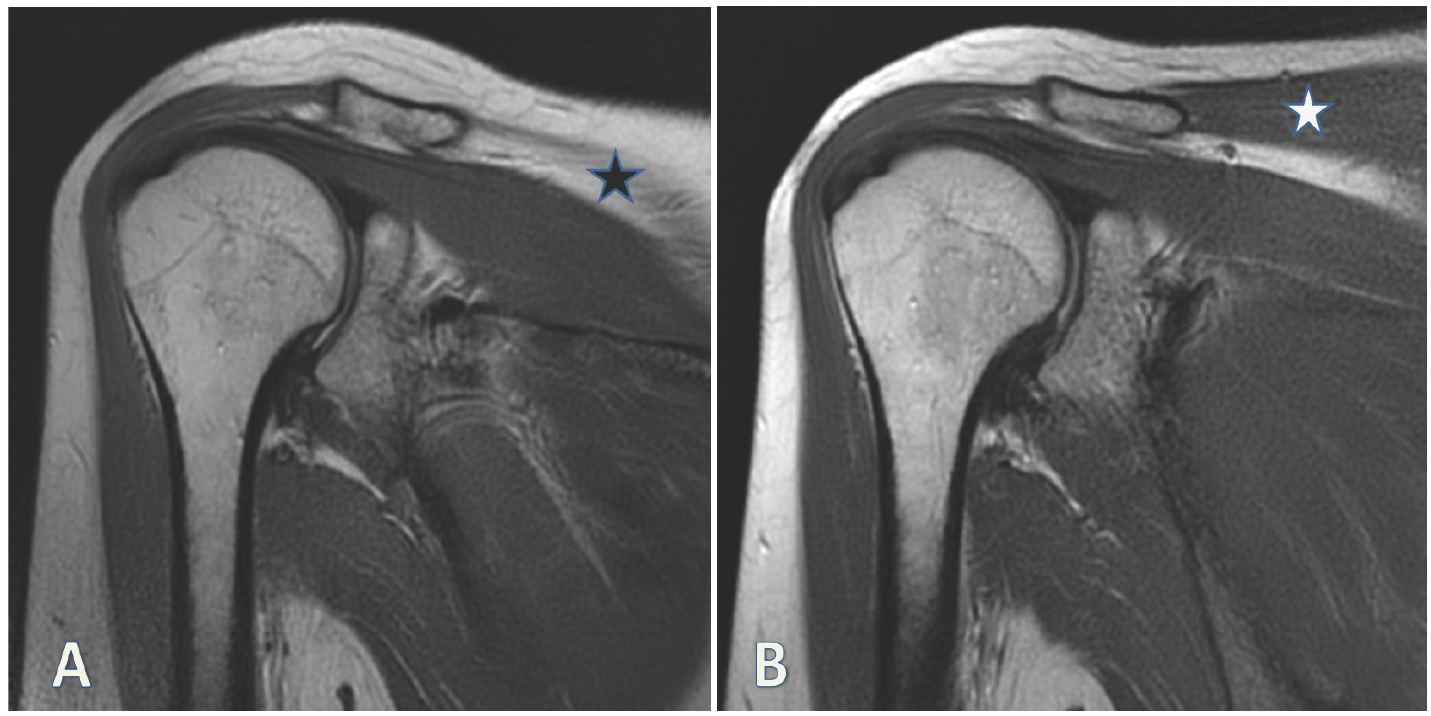
Left side (A) and right side (B) MRI images showing trapezius muscle (asterisk = trapezius muscle).
Discussion
Shoulder pain that radiates to the arm and scapula is seen in serratus anterior palsy. Patients often complain of shoulder weakness. Medial scapular winging is generally evident at rest, as the scapula shifts more medially and upward compared to the intact side. With active flexion of the arm or wall push, the position of the scapula becomes more evident. In trapezius palsy, patients experience shoulder pain, loss of strength in the shoulder girdle, and asymmetrical neckline due to drop shoulder. Typically, winging is minimal, pronounced during arm abduction, and the upper angle of the scapula shifts more laterally from the midline of the body when compared to the lower angle. Scapular winging may disappear during the elevation of the arm. In rhomboid palsy, pain is observed in the medial border of the scapula, which can spread to the lateral side of the arm and forearm. There is a very mild winging of the scapula, especially in the inferior angle that has shifted laterally [5]. DSN palsy is best demonstrated by slowly lowering the arms from the forward-raised position [6].
The most common cause of SAN lesions is iatrogenic injury during operations on the posterior cervical triangle of the neck [5,7]. However, a SAN injury can develop due to various traumatic causes, such as stretch injury, traction injury, penetrating injury, and blunt trauma [8]. Trapezius paralysis can cause shoulder pain, limitation in arm abduction above 90° scapular winging, and shoulder drop [7,8]. During the anatomical course of the DSN, it often pierces the middle scalene muscle, and in the case of hypertrophy of the middle scalene muscle, the DSN can often be trapped here. The DSN can also be injured as a result of repetitive overhead activities while doing work and sports or, in some patients, as a result of carrying heavy loads or chronic extreme stress due to poor posture, or after iatrogenic (postoperative) or vehicle accidents [9]. Patients with DSN lesions usually have shoulder pain along the medial border of the scapula, which sometimes radiates to the C5 and C6 dermatomes. When the arm is lifted over the head, the WS appears. Hypotrophy and weakness develop in both the rhomboid and levator scapula muscles [10]. It is difficult to diagnose the WS associated with the DSN lesion because the rhomboid muscles are anatomically located deeper under the trapezius muscle and, in addition, the scapular winging is mild. Some authors have suggested that DSN palsy is an underdiagnosed cause of shoulder pain due to this difficulty [5]. Desong et al. demonstrated that 25 of 36 patients were initially misdiagnosed with neurosis, trapezius myalgia, cervical spondylosis, and adhesive capsulitis [11].
In this case, when the EMG report carried out at the outside center was examined, it was found that only the SAN was evaluated from the nerves that may cause WS. The patient complained of pain radiating to the shoulder and lateral part of the arm, starting from the medial border of the scapula. After active flexion and abduction of the patient’s arm, the inferior angle of the left scapula was found more laterally displaced than the left superior angle. Due to the typical radiation of pain and position of the scapula, rhomboid muscle strength was evaluated with suspicion of rhomboid palsy. The patient’s left shoulder and periscapular muscles were evaluated with US for muscle thickness since the rhomboid muscles were weak. It was observed that the left trapezius muscle and left rhomboid major muscle below were atrophic compared with the right side. US evaluation showed an increase in echodensity on the left side in the rhomboid major and especially the trapezius muscles (Figure 2). It was thought that a DSN lesion may accompany a SAN lesion because the thickness of the left rhomboid major muscle was significantly lower than the right side. Right and left trapezius muscle thicknesses were measured as 3.5 and 2.2 mm, respectively. Right and left rhomboid muscle thicknesses were measured as 7 and 3.1 mm, respectively.
In the acute period of the peripheral neuropathy, muscle hypertrophy and edema can be seen. Muscle atrophy will not occur in acute injuries. If recovery is insufficient, in chronic peripheral neuropathies, motor units may be lost. Muscle tissue is replaced by fat and fibrous tissue so atrophy occurs. As a result of this, the muscle appears white on ultrasound. In the case of a suspected focal peripheral neuropathy, the affected muscle can be compared with the intact muscle on the opposite side via ultrasound. Measurement of muscle atrophy with ultrasound can only be used in the diagnosis of chronic peripheral nerve lesions. In addition, ultrasound allows nerves to be viewed directly [12]. Atrophy seen in the muscle indicates the loss of function in the nerve. Simon et al. [13] have shown that denervated hand muscles have significantly reduced thickness and significantly increased echogenicity on ultrasound compared with intact muscles [13]. The SCM and trapezius muscles innervated by the SAN were evaluated by US. While the SCM muscles of both sides were measured with similar thickness (Figure 3), atrophy was detected in the left trapezius muscle. These US findings suggested that a traumatic nerve lesion developed in the segment of the SAN after innervating the left SCM. The EMG study also supported the US findings.
Conclusion
Musculoskeletal ultrasound (MSUS) can be used as an aid to EMG study in the diagnosis of unilateral chronic peripheral nerve lesions by measuring muscle thickness, and perhaps, it may be conceivable to use MSUS as an alternative technique in cases that cannot tolerate EMG. Since there may be a single peripheral nerve lesion or more than one reason in the etiology, EMG evaluation and physical examination should be done completely and very carefully.



