Introduction
Background
Breast cancer is the most frequently diagnosed and leading cause of death in women.(1) Over the recent past, there has been an increase in the number of women electing contralateral prophylactic mastectomy (CPM) in unilateral breast cancer.(2) In 2018, breast cancer ranked first in the number of new cases and third in the number of deaths in South Africa. The International Agency for Research on Cancer reported 14,097 new cases and a 5-year prevalence of 37 662 people across all ages.(3)
In developing countries, rapid societal and economic changes are potential reasons for lifestyle trends to shift towards those in high-income countries.(4) These lifestyle trends have led to an increase in the burden of cancers associated with reproductive, dietary, and hormonal factors such as breast cancer.(4)
In women who are diagnosed with unilateral breast cancer, the risk of developing contralateral breast cancer is three to five times higher than those women who do not have breast cancer, with even higher risk in women with either BRCA1 or BRCA2 gene mutations.(5) Tumour suppressor genes, BRCA1 and BRCA2 germline mutations pose the most significant risk factor for breast and ovarian cancer.(6) The lifetime risk of contralateral breast cancer is 40-65% in women with this mutation, and it is in this demographic that CPM has the most significant potential benefit.(7) Elsayegh et al. explored the benefit of CPM in women with unilateral breast cancer and a germline BRCA1/2 mutation. They found that the risk of developing metachronous contralateral cancer was reduced by 91%.(10) The reported tumour characteristics associated with increased CPM rates have been a clinically higher tumour stage, multicentric primary tumour, invasive and in situ lobular histology and recent year of diagnosis.(8)
In women without a known predisposition, the annual risk of metachronous development of clinically detected contralateral breast cancer is about 0.6%.(9) In the United States, in women of all ages, the rate of CPM increased from 1.9% in 1998 to 10.2% in 2011 and much higher rates in women under 45 years of age, rising from 3.7% in 1998 to 26.2% in 2011.(9) These rates appear to be out of proportion to the reported risks of metachronous cancer.(9)
Several reports have identified demographic, histopathological/oncological characteristics and psychological factors of patients who chose CPM in unilateral breast cancer. Factors identified from these three distinct but often overlapping groups are summarised in Table 1. A fourth factor of cosmetic symmetry may also be important in some patients.
| Demographic | Histopathological/Oncological | Psychological |
|---|---|---|
| Young age (<45) (8–11) | Stage 1-2 (4,9,12–15) | Fear of recurrence (13,16–18) |
| White (8–11,13,14) | Invasive lobular (8,9,11–13) | Perceived benefit (16,17) |
| High Socio-Economic Status (9,12,13) | Small tumour size (<2 cm) (10) | Influence by family/friends (17,18) |
| Family History (7,10,13) | Node negative (10) | Over-estimation of risk (16,17,19) |
| ER/PR negative (10) | ||
| Radiation (10) | ||
| First primary tumour (10) | ||
| Neoadjuvant chemotherapy (12,15) | ||
| BRCA 1/2 (12,13) |
The increase in the trend for CPM was also studied by Agarwal et al., who found a 3.5-fold increase from 1997 to 2005, with young age, family history, White ethnicity and the availability of immediate reconstruction being predictors of this choice.(10) Furthermore, it was found that the odds of CPM were independently increased by later years of diagnosis, lower stage, smaller tumour size, node-negative status, first primary cancer, higher median county income and a higher percentage of women with greater than 12 years of education. Among patients who underwent breast reconstruction, younger age, White race, and later year of diagnosis had higher odds of CPM.(10)
Similarly, a 2015 report from the National Cancer Data Base in the USA found that a higher proportion of White women fell into a higher socioeconomic group, 15% more likely to have private medical insurance and thus more likely to choose CPM compared to their lower socioeconomic status counterparts who were predominantly Black, Asian and Hispanic.(9)
Lizarraga et al. explored the risk of developing contralateral breast cancer by assessing specific demographics and tumour characteristics.(20) This particular breakdown is essential as it indicates to the health professional whether the patient choosing the procedure is justified in their reasons outside of the genetic risk and thus aids in the counselling, advice, and reassurance. They found that in the absence of genetic mutations, patients younger than 35 years with a strong family history and with oestrogen receptor-negative tumours have a higher incidence of contralateral breast cancer.(20) Also, White women were more likely to choose CPM than Black women.
Covelli's group questioned women on the psychological aspects of their breast cancer diagnosis. All the patients reacted to the news of the diagnosis with shock and fear. The women said that despite being counselled that breast-conserving treatment versus unilateral mastectomy was equivalent in terms of long-term survival, they felt that the odds of survival were increased if all the breast tissue was gone. Women who were non-carriers of the genetic mutation, when answering a questionnaire, estimated the 5-year risk of contralateral breast cancer at 15% (instead of 0.6 %).(9) This misconception led to an increase in the choice of CPM.(16)
The modern patient has increased access to information, which expands the influence in the decision-making relating to their disease. A recent study showed that patients were mainly influenced by breast surgeons, plastic surgeons and medical oncologists rather than TV, the internet, articles and magazines.(21)
Determining the reasons behind the trend for choosing CPM is vital to address potential issues in patient counselling and peri-operative support in the future. Long-term survival after breast cancer means that surgical decisions have long-lasting consequences for patients. There is no data in South Africa on the oncological and demographic factors influencing the decision to choose CPM. This study thus aimed to ascertain characteristics in patients with unilateral breast cancer who chose CPM.
Methods
Study design
The study was a retrospective, descriptive study of patients undergoing mastectomy for unilateral breast cancer, comparing those choosing UM with those choosing mastectomy with CPM as well. A record review of enrolled participants’ histological results and demographic details was conducted at the Breast Care Clinic of Helen Joseph Hospital, a medium-sized public hospital in Johannesburg, South Africa. The patient details and chosen surgery information were captured prospectively in the Breast Care Clinic database at the time of diagnosis.
Data acquisition
Female patients of all ages who underwent a mastectomy for unilateral breast cancer from 2013 to 2015 were included in the study.
The hospital's billing system, the Uniform Patient Fee Schedule (UPFS) or “H” status, is the same that is used for all public sector hospitals in South Africa.(22) Patients are classified as full-paying or subsidized patients. The default classification for a person without income is H1. Subsidization depends on the assessment of income by the means test. We used “H” status as an indicator of socioeconomic status based on a patient's ability to pay the hospital fees. The patients fell into either H0, H1 or H2.(22)
Each patient's pathology report was retrieved from the National Health Laboratory System's ‘Labtrak’ system. The information recorded included the following: number of specimens received; weight of the breast (in the case of two breasts, the CPM breast was recorded); histology of the CPM side; use of neoadjuvant chemotherapy; stage of breast cancer.
Statistical analyses
The data was captured in Microsoft Excel and exported into SPSS (Statistical Product and Service Solutions) software for data analysis. Descriptive statistics are reported as appropriate, including frequencies and percentages, means and standard deviations (SD) or median and interquartile ranges (IQR). The Mann-Whitney U test assessed whether the median age and weight differed significantly between the UM or CPM groups. The Chi-square or Fisher's Exact test of association was used, as appropriate, to determine associations between categorical variables according to UM or CPM groups. A p-value less or equal to 0.05 was considered statistically significant. Ethical approval for the study was obtained from the University of the Witwatersrand Human Research Ethics Committee (Medical).
Results
A total of 299 patients had mastectomies for unilateral breast cancer during the study period, of whom 59 (19.7%) had CPMs. The demographic and clinical information, including age, race, ‘H’ status and breast weight, are summarised in Table 2. There was a significant difference in the age of patients choosing unilateral versus CPM, with the UM patients being significantly older than the CPM patients (p = 0.03). Most patients were of low socioeconomic status (H1: 92.3%) (Table 2). Significantly more Black patients were classified as H1 compared to the other races at 96.5% vs 86.7%, respectively (p = 0.003). However, there was no difference in the H status of patients between the UM and CPM groups.
| Parameter | All (n = 299) | UM (n = 240) | CPM (n = 59) | P-value |
|---|---|---|---|---|
| Age (years), median (IQR) | 56.0 (44.0 – 65.0) | 56.0 (45.5 – 66.0) | 53.0 (41.0 – 62.0) | 0.03* |
| Breast weight (grams), median (IQR) | 586 (371–933) | 577 (355-860) | 655 (462-1020) | 0.09 |
| Race, n (%) | (n = 298) | |||
| Black | 170 (57.1%) | 152 (63.6%) | 18 (30.5%) | <0.001** |
| Coloured | 43 (14.4%) | 35 (14.6%) | 8 (13.6%) | |
| Indian | 16 (5.4%) | 13 (5.4%) | 3 (5.1%) | |
| White | 69 (23.2%) | 39 (16.3%) | 30 (50.9%) | |
| H Status, n (%)*** | ||||
| H0 | 22 (7.4%) | 17 (7.1%) | 5 (8.5%) | 0.82 |
| H1 | 276 (92.3%) | 222 (92.5%) | 54 (91.5%) | |
| H2 | 1 (0.3%) | 1 (0.4%) | 0 (0%) |
Abbreviations: IQR, interquartile range; CPM, contralateral prophylactic mastectomy; UM, unilateral mastectomy.
Mann-Whitney U test.
Chi2/Fisher's exact test.
“H” status as an indicator of socioeconomic status based on the ability to pay the hospital fees, the patients fell into either H0, H1 or H2.
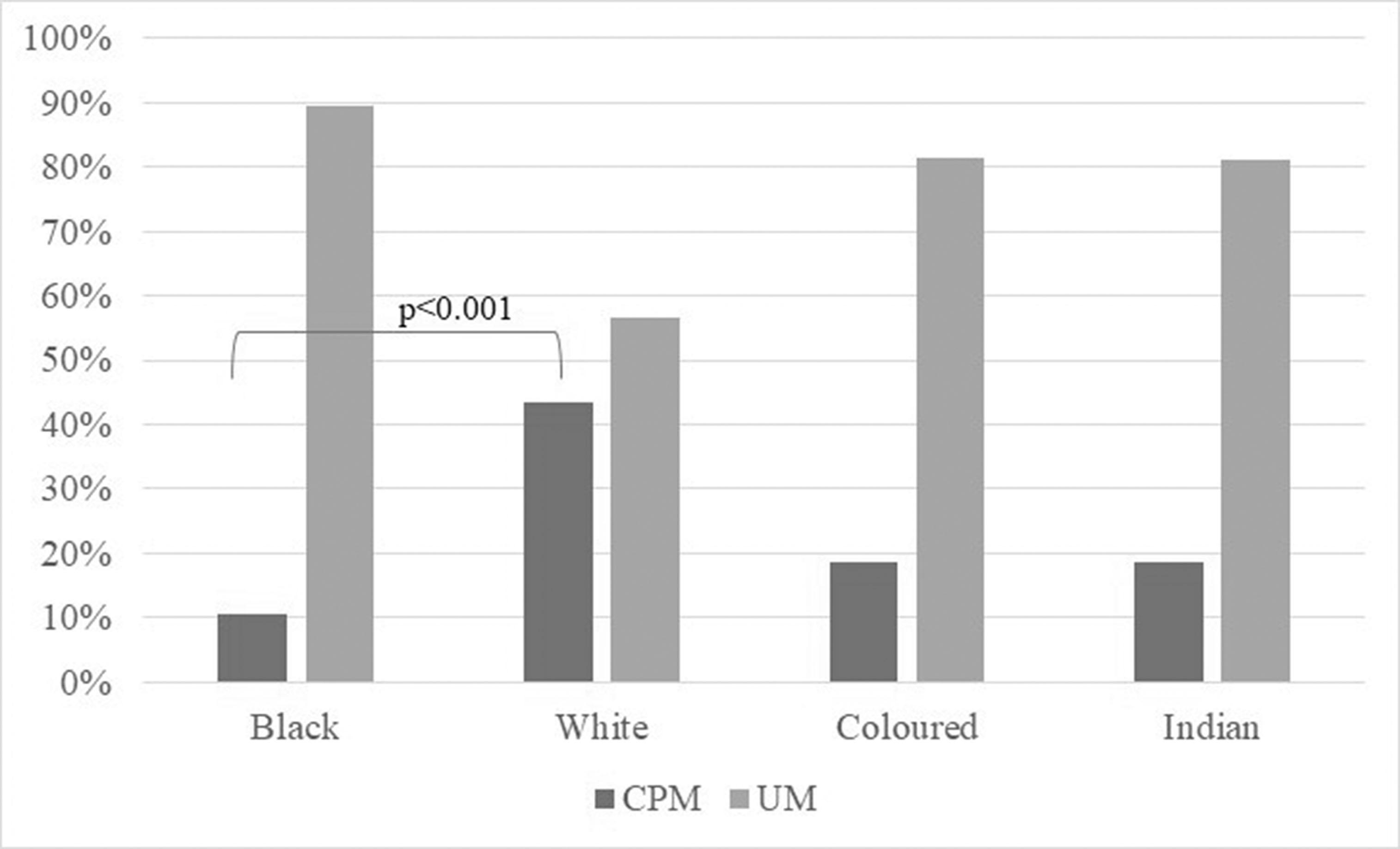
The majority of patients in the study were Black (57.1%), followed by White (23.2%), Coloured (14.4%) and Indian (5.4%) patients. One patient's race was not documented. Overall, there was a highly significant difference in patients who chose UM vs CPM across racial groups (p♯αμπ;λτ;0.0001). (Figure 1) Specifically, only 10.6% of Black patients chose CPM compared to 43.5% of White patients (Bonferroni corrected p-value♯αμπ;λτ;0.001). Women who underwent CPMs had a trend for a larger median weight of the breasts, although this did not reach statistical significance (p = 0.09).
The histopathology of the breasts, including breast weight, primary tumour histology, histology of the contralateral side and TNM staging of the tumour, is shown in Table 3. One patient's histopathology was not captured, and only 211/299 patients had data on neoadjuvant therapy.
| Parameter, n (%) | All (n = 298) | UM (n = 239) | CPM (n = 59) | P-value |
|---|---|---|---|---|
| Histology of tumour | ||||
| Ductal Carcinoma In Situ | 18 (6.0) | 15 (6.3) | 3 (5.2) | |
| Invasive Ductal Carcinoma | 230 (77.2) | 184 (76.7) | 46 (79.3) | 0.69 |
| Invasive Lobular Carcinoma | 10 (3.4) | 7 (2.9) | 3 (5.2) | |
| Other subtypes | 40 (13.4) | 34 (14.2) | 6 (10.3) | |
| Histology of CPM | ||||
| Ductal carcinoma in situ | 1 (1.7%) | - | 1 (1.7%) | - |
| No Invasive Malignancy | 47 (81.0%) | - | 47 (81.0%) | |
| NA* | 10 (17.2%) | - | 10 (17.2%) | |
| TNM stage | ||||
| Stage 0-2a (early) | 129 (43.3%) | 98 (41.0%) | 31 (52.5%) | 0.14 |
| Stage 2b-4 (late) | 169 (56.7%) | 141 (59.0%) | 28 (47.5%) | |
| Neoadjuvant chemotherapy | n = 211 | |||
| Yes | 161 (76.3%) | 133 (54.7%) | 29 (49.2%) | >0.99 |
| No | 50 (23.7%) | 42 (17.3%) | 9 (15.3%) |
Abbreviations: CPM, contralateral prophylactic mastectomy; UM, unilateral mastectomy.
This applies to the unilateral mastectomy patients
There was no significant association between the UM or CPM group for each of the following variables: Histology of tumour (p-value = 0.69), TNM stage (p-value = 0.14) and neoadjuvant chemotherapy (p-value >0.99).
The population with CPM were predominantly White, with the mean weight of the breast being larger than that of the UM counterparts and the median age being younger. Pathologically, most of the population had invasive ductal carcinoma, were T2 N +, thus either Stage IIb or IIIa, and had had neoadjuvant chemotherapy. Of this group, only one patient was found to have a contralateral malignancy.
Discussion
International trends influence patients’ decision-making from both a patient's and a health professional's point of view. In the era of increased access to information, health professionals must not be deterred from practising evidence-based medicine. There always, however, lies a caveat to applying blanket medical advice to diverse communities.
The Department of Health provides public and private health services in South Africa. Citizens who access the public health service are of a lower socioeconomic standing.(23) Adequate, evidence-based health care is provided to all patients despite their socioeconomic status. The need to stratify patients according to ‘H’ status allows them to be billed according to their affordability. In this study, we did not expect to see a discrepancy between the UM and CPM populations based on socioeconomic standing, as the majority of this population is of similar economic standing.
International studies have shown that White women were more likely than any other race to have CPM. This finding was also demonstrated in our study. The varying levels of education and access to information among the patients could influence this. Owing to the country's Apartheid history, significant discrepancies in equality still exist. The country's White population had access to better education and health care before establishing democracy.(23) Despite only 23.2% of White women in the study population, more than half the CPM procedures were performed in this group (50.9%). It is, however, possible that there are also other culture-specific influences that this study does not elicit from the various ethnic groups.
We hypothesized that women with larger breasts would more likely choose a CPM procedure. Despite the CPM group having a larger median breast weight, this did not reach statistical significance. This finding is consistent with the literature that did not find this factor influential on CPM choice.
A higher percentage of patients post neoadjuvant chemotherapy still opted for UM, which, although not statistically significant, is inconsistent with international studies which demonstrated neoadjuvant chemotherapy as a factor favouring CPM.(12,15)
The cancer stage at presentation was higher in our study than in the rest of the world.(24) Furthermore, a high percentage (56.7) of patients were found to have late-stage (2b–4) breast cancer. It can, however, be noted that the population that underwent CPM mastectomies had the highest percentage early stage (stage 0-2a) compared to the late stage (stage 2b-4). This finding is consistent with previous reports showing that lower-stage tumours were present in patients who had chosen CPM.
The most prevalent histology of the total population was invasive ductal carcinoma, which was reflected in both CPM and UM procedures. Previous studies, however, have reported that patients choosing CPM had invasive lobular carcinoma as the prevalent histology. The incidence of contralateral breast cancer is higher for invasive lobular carcinoma, and thus, the preservation of the contralateral breast is less frequent.(25) In the current study, only 30% of patients with invasive lobular carcinoma had a CPM, suggesting that the biology of the tumour did not play a significant role in influencing the decision to undergo CPM. This finding may be related to the fact that the health practitioner, in line with the ethical considerations of the evidence, would not routinely advise CPM, even in discussing the risk of contralateral involvement of invasive lobular carcinoma.(26)
A history of neoadjuvant chemotherapy has been associated with electing CPM. In this study, the analysis of this factor was limited because almost 30% of the study population did not have the timing of their chemotherapy documented. Of the patients where it was reported, 76% had neoadjuvant chemotherapy, and in this group, unlike the trend in international literature, only a small percentage (17.9%) had CPM. This rate is similar to the group who underwent CPM without neoadjuvant chemotherapy (17.6%).
Limitations of the Study and Alternative Approaches
The limitations in the study arose from incomplete file records. In the public sector, there are significant limitations to the assessment of the socio-economic status of a patient based on UPFS, or ‘H’ status, as the latter is based on the evaluation of income, which in turn is difficult to accurately verify on admission to the hospital. Even though the setting of this study was an urban clinic, rural patients may have unwittingly been included as they often travel far due to the increased access to healthcare in urban areas; this may have impacted their H-status.
Conclusion
The demographic and histopathological characteristics of breast cancer which influence the choice of CPM in the South African context have some similarities to those in the international literature in that White and younger women more often choose CPM compared to other racial groups. In future, with the continuation of monitoring of our patients’ characteristics, increasing access to information, and advances in breast cancer detection and management, the decision to choose CPM may no longer carry a racial bias. Of concern is the more advanced stage of breast cancer at presentation in our study as compared to international studies. Public health awareness and screening measures need to be strengthened significantly, especially for the indigent population that relies solely on the public healthcare system in South Africa.
All authors have contributed as stipulated by the authorship guidelines. There are no conflicts of interest to declare, and the study did not require funding.

