1. INTRODUCTION
A uterine leiomyosarcoma (ULMS) is a rare malignant tumor of the smooth muscle cells that accounts for approximately 1.3% of all uterine malignancies. A ULMS is a type of uterine sarcoma that accounts for approximately 45% of all uterine sarcomas. The malignancy rate is high and a ULMS is prone to distant metastasis and recurrence in the early stages. Therefore, the prognosis is poor with a 5-year survival rate of only 20%-30% [1]. A ULMS is more common in the uterus than the cervix. A ULMS can originate from the smooth muscle of the uterus or may occur secondary to a malignant leiomyoma. Furthermore, a ULMS is more common in women 40–60 years of age and has clinical manifestations like uterine fibroids, including abdominal pain, abdominal and pelvic masses, and abnormal vaginal bleeding. The only effective treatment for a ULMS is complete early resection. There is no established adjuvant chemotherapy regimen after a complete resection, rendering adjuvant radiation therapy ineffective. Chemotherapy is the primary treatment for unresectable, advanced, and recurrent tumors [2].
2. CASE DESCRIPTION
A 47-year-old female was admitted to the hospital because of “paroxysmal abdominal pain for 6 months that worsened for 1 day.” Six months earlier the patient had no apparent cause for diffuse abdominal pain, which is paroxysmal and relieved after self administration of ibuprofen. No other imaging examinations were performed before admission to the hospital. Initially, the pain was described as a stabbing sensation in the lower left abdomen, which gradually developed into widespread abdominal pain, accompanied by paroxysms of colic and nausea but no vomiting. The physical examination revealed abdominal distension, tenderness in the middle and lower abdomen, and a palpable mass approximately 20 cm × 10 cm in size around the umbilicus and lower abdomen. The mass had a textured surface and clear boundaries, extended into the pelvic cavity, and presented as voiced sounds on percussion. The uterus was shown to be significantly enlarged, with irregular, mixed-density soft tissue internal masses visible on plain computed tomography (CT) scan. Cystic and necrotic areas with indistinct boundaries were visible (Figure 1a). The enhanced mass was uneven and significantly enhanced with strip-like enhancement shadows. The cystic and necrotic areas were not significantly enhanced (Figure 1b). Enlarged metastatic partially fused lymph nodes were noted in the abdominal cavity and retroperitoneum; the degree of enhancement was similar to that of the primary tumor (Figure 2a, b). The uterine space occupying lesion was suspected to be a malignant tumor with local bleeding, necrosis, and multiple metastases to the abdominal and retroperitoneal lymph nodes. A large mass was observed in the lower and middle parts of the abdomen intraoperatively. The large mass in the abdominal and pelvic cavities was shown to be a uterine mass with bilateral adnexal lesions, approximately 20 cm × 20 cm × 15 cm in size. The bilateral retroperitoneal masses were palpable. The left- and right-side masses were 6 cm × 6 cm × 6 cm and 8 cm × 6 cm × 6 cm in size, respectively. A total hysterectomy, left salpingectomy, right adnexectomy, and resection of the retroperitoneal mass were performed. The pathologic diagnosis was a ULMS with bleeding and necrosis (Figure 3a, b). Due to missing patient information, the postoperative outcome is unknown.
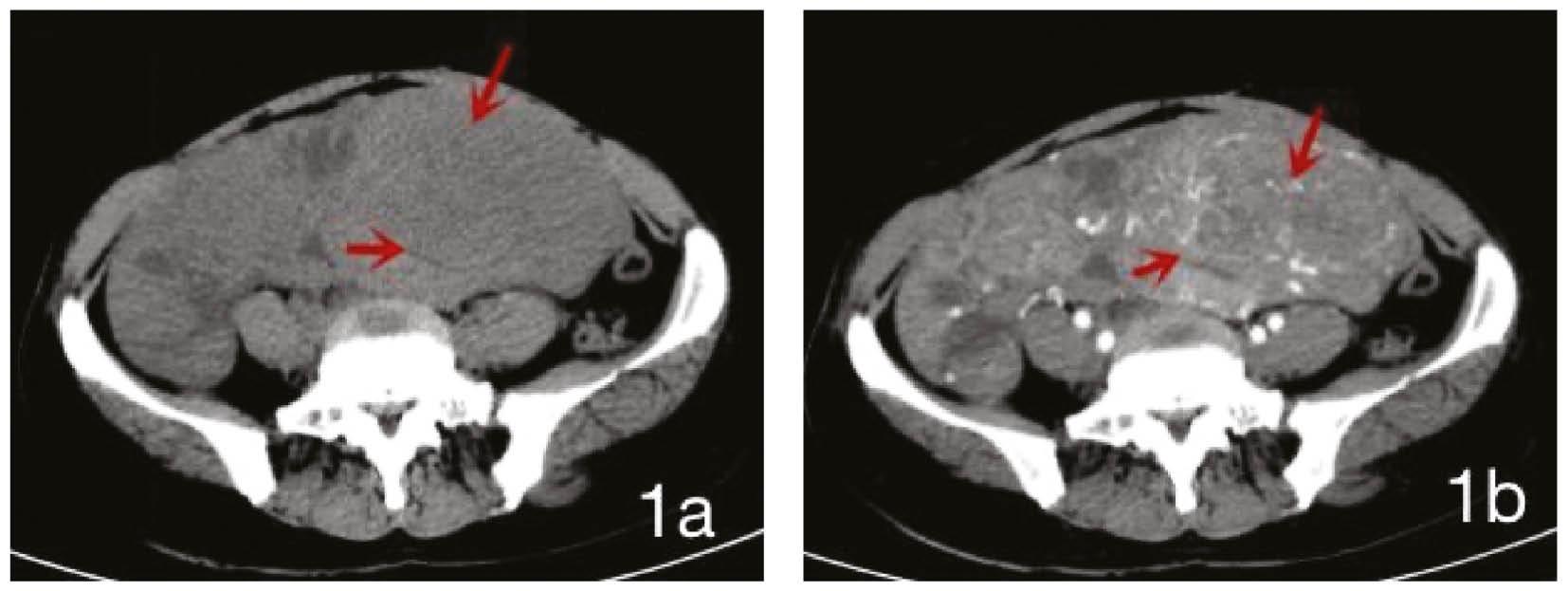
(a) CT plain scan shows a mass shadow (long arrow) connected to the uterus (short arrow), with a lower density necrotic area visible inside and a clear boundary with surrounding tissue; (b) The enhanced mass was unevenly enhanced and no enhancement was observed in the cystic necrotic area.
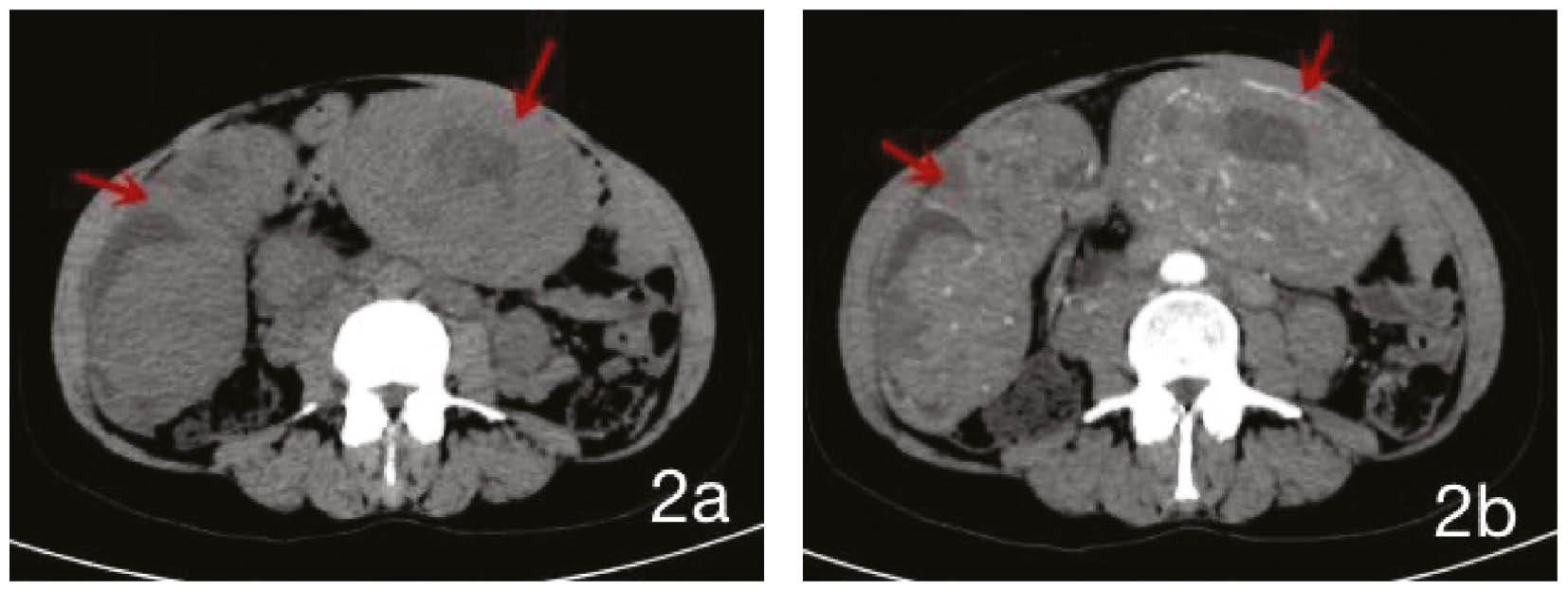
(a, b) Multiple masses of varying sizes were present in the abdominal cavity with uneven enhancement. There was no significant enhancement in the necrotic area of the internal capsule. Enlarged, partially fused lymph nodes were noted in the abdominal cavity and retroperitoneum. The degree of enhancement was very similar to the uterine mass imaging, indicating retroperitoneal metastatic lymph nodes in the abdominal cavity.
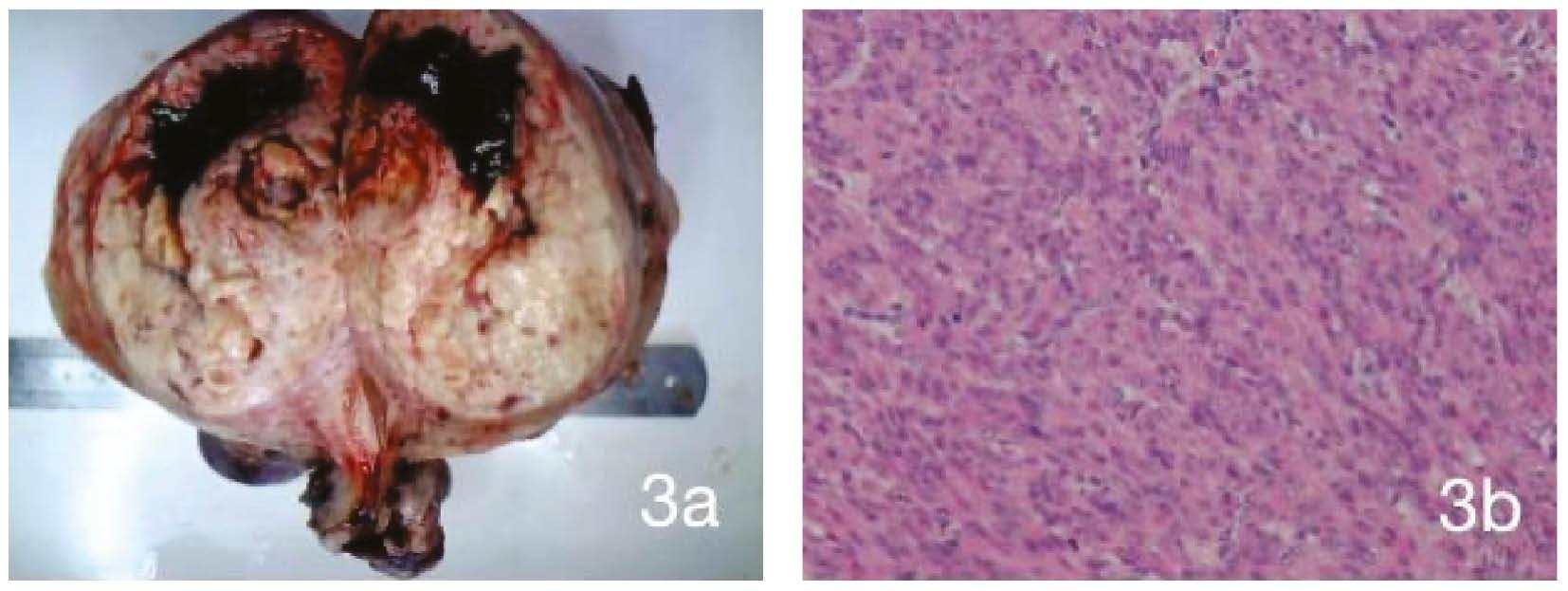
Uterine leiomyosarcoma with bleeding and necrosis.
(a) Giant mass in the abdominal and pelvic cavities, approximately 10 cm × 9 cm × 6 cm in size with an intact capsule, indicating a nodular shape. The cut surface was gray-white, solid, soft in texture, with local bleeding, showing a lobulated shape; (b) HE × 400, the tumor was composed of spindle-shaped, dense cells with obvious cell dysplasia and visible nuclear division. Immunohistochemical staining revealed the following: SMA(+); Desmin(+); ER(+90%); Ki-67(+10%); PR(+90%); S-100(−); CD117(−); and CD34(−).
3. DISCUSSION
The cause of uterine leiomyosarcoma (ULMS) is unknown and may be related to low expression of estrogen receptors (ER) and progesterone receptors (PR); the Ki-67 gene related to cell proliferation is positive;tumor suppressor genes P53, P16, and apoptosis regulatory gene Bcl-2 are highly expressed, and the MED12 gene mutation is associated with different types of MicroRNA [3] expression. The immunohistochemistry of this patient is consistent with the above description.
The patient was 47 years of age and presented with paroxysmal abdominal pain and irregular vaginal bleeding, both of which were consistent with her age and the clinical characteristics of a ULMS. CT is a common diagnostic imaging method for uterine diseases. A plain CT scan can visually display the size and location of tumors. Because of the similar features of many pelvic tumors and ULMSs, it is difficult to distinguish ULMSs from other pelvic tumors based solely on plain CT scans. Therefore, further differentiation is needed through enhanced scanning because tumors have different enhancement methods; specifically, uterine fibroids have mild-to-moderate enhancement after enhanced scanning. Enhanced scanning of endometrial cancer often results in mild enhancement and the degree of enhancement is less than the adjacent uterine muscle layer. An enhanced scan of uterine adenomyosis shows uneven and patchy enhancement. In contrast, an enhanced scan of ULMS shows uneven and significant enhancement of the tumor and clearly displays retroperitoneal metastatic lymph nodes, which are also the enhanced features of a ULMS. A previous CT diagnosis of ULMS showed uterine enlargement with a large uneven density mass in the uterine cavity containing calcified spots. After enhancement, the mass showed uneven and significant enhancement in the arterial phase, continuous enhancement in the venous phase, uneven enhancement of the uterine muscle layer, and destruction of the left posterior wall. Compared to the previous diagnosis of a ULMS, the patient presented herein had similar plain CT scan findings and enhanced features. At the same time, a ULMS can be differentiated based on clinical manifestations. For example, uterine fibroids often have no obvious clinical manifestations and are often incidental findings during physical examination. Adenomyosis of the uterus is characterized by refractory dysmenorrhea and progressive worsening, and the size of the lesion can change during the menstrual cycle. The most apparent manifestation of a ULMS is that the lesion grows significantly in the short term, such as doubling in size over 6 months. Hence, the rapid growth of postmenopausal uterine fibroids is a major indication of possible sarcomatosis in clinical practice and is also a characteristic that warrants clinical vigilance. Ultrasound is the preferred examination method in gynecology and has diagnostic value. However, Liu et al. [4] studied 16 patients confirmed to have ULMSs based on a puncture or surgical pathologic diagnosis. Based on the pathologic diagnosis results, a review of preoperative ultrasound images showed that only a small number of cases were correctly diagnosed with uterine malignant tumors, while the majority of cases could not be clearly diagnosed and were misdiagnosed as benign uterine leiomyomas. When the tumor volume is large, organs undergo significant displacement and deformation. The original anatomic position and typical shape are lost, and the relationship and location between the tumors and organs become inaccurate, making the differential diagnosis difficult. However, CT can track blood vessel flow, reconstruct large blood vessels and their branches, demonstrate the relationship between blood vessels and tumors, and improve the accuracy of tumor localization and diagnosis. An accurate preoperative imaging diagnosis can assess the size and location of the tumor, and show whether there is adjacent invasion and distant metastasis, which is beneficial for clinical staging and surgical decision-making. Furthermore, an accurate preoperative imaging diagnosis improves the surgical success rate and favorably impacts prognosis. Paik et al. [5] concluded that the most important prognostic factor for the survival of patients with a ULMS is tumor staging at the time of diagnosis. Long et al. [6] reported a case of preoperative CT three-dimensional reconstruction-assisted surgical treatment for metastatic ULMS of the vena cava. Studies have shown that magnetic resonance imaging (MRI) is more sensitive than CT in distinguishing the nature and origin of pelvic masses. MRI has high soft tissue resolution, and sagittal, coronal, and cross-sectional imaging clearly shows various anatomic bands of the uterus, which demonstrates the clear relationship between the tumor and surrounding organs. MRI has high diagnostic value for the localization and qualitative diagnosis of uterine tumors. MRI can utilize multi-parameter characteristics, such as reflecting the degree of malignancy through the value of the apparent diffusion coefficient in diffusion weighted imaging. Although there is ambiguity in the diagnostic accuracy of individual characteristics, MRI is still the preferred imaging method for in-depth evaluation of uterine fibroid tumors and depicting the local spread of malignant diseases [7]. Compared to MRI, the main advantage of CT scanning is that CT is less expensive and easier for patients to accept [8].
A ULMS has symptoms and signs like common uterine leiomyomas, making the preoperative differential diagnosis difficult, with a high misdiagnosis rate, early metastasis, and unsatisfactory treatment results. Women >40 years of age should undergo regular physical examinations. If symptoms, such as abdominal pain, irregular vaginal bleeding, or postmenopausal vaginal bleeding, occur patients should seek medical attention in a timely manner. Patients diagnosed with uterine fibroids should pay close attention to the possibility of developing a ULMS if the examination reveals rapid growth of uterine fibroids over a short period of time [9]. The comprehensive use of diagnostic curettage, ultrasonography, CT, and MRI can significantly improve the ULMS diagnostic rate. However, owing to the histologic correlation between a ULMS and other uterine tumors, further in-depth research is warranted for the early diagnosis of a ULMS.

