| What is the scientific question being addressed? |
| To provide expertise on the optimal timing and surgical techniques for managing patients with aortic annular involvement due to infective endocarditis. |
| What is the main novel finding? |
| In patients with a large residual lumen in the left ventricular outflow tract (LVOT) or in the acute infectious phase, perforating the left ventricular side during valve annulus reconstruction can prevent aortic root abscess formation and enhance the efficacy of local antibiotic therapy. |
Infective endocarditis (IE) is a serious infection caused by pathogenic bacteria that travel through the bloodstream and colonize the endocardium, thus resulting in rapid progression, numerous complications, and high mortality [1]. Despite the emergence of new diagnostic and therapeutic strategies, the 1-year mortality rate has not improved and remains at 30% [2]. Surgical management of IE involving the aortic annulus is critical, because pharmacologic therapy alone is usually insufficient to address the structural damage and hemodynamic instability caused by this severe infection. The goals of surgical intervention are eradicating the foci of infection, repairing or replacing the damaged valve, and restoring the integrity of the aortic root [2, 3]. The aim of this article was identifying the most effective surgical treatment for aortic annular involvement due to IE by reviewing the literature and analyzing the past 5 years of treatment experience in our department.
A total of 21 cases of IE involving the aortic annulus in patients admitted to our department between October 2017 and December 2022 were analyzed. The cohort included 13 males and 8 females, with a median age of 41 years (range: 14–72 years). The median disease duration was 2 months (range: 7 days–4 months), and the median follow-up period was 3.3 years (range: 1.5–6.2 years). In this cohort, 11 patients had underlying heart disease, including six cases of rheumatic valvular heart disease, three cases of congenital bicuspid aortic valve, and two cases of congenital heart disease with intracardiac shunting. Blood cultures indicated Staphylococcus in 47.62% (n = 10), Streptococcus in 19.0% (n = 4), Enterococcus in 14.3% (n = 3), and negative findings in 19.0% (n = 4) of cases.
All patients underwent cardiac surgery under hypothermic cardiopulmonary bypass. Three cases required emergency surgery because of severe ventricular arrhythmia, and uncontrollable heart failure combined with infection, whereas the remaining cases underwent elective procedures. The surgical procedure involved complete resection of the diseased aortic valve leaflets and aortic annulus, with the extent of annular resection determined according to the degree of local infection, to ensure that at least 3 mm of normal tissue was excised. For patients with disrupted aortic-mitral fibrous continuity, reconstruction was achieved with a biopatch. In patients with acute infection or remnant cavity formation in the aortic root, perforations were made in the biopatch on the left ventricular side of the reconstructed annulus. Furthermore, aortic valve replacement was performed with interrupted sutures on the reconstructed valve annulus, and most gaskets were placed on the aortic side. Concurrent cardiac malformations were addressed simultaneously. All patients underwent outpatient follow-up after discharge, during which time their cardiac function class, quality of life, and clinical status were documented at each visit.
The aortic annulus was reconstructed in 16 patients: complete reconstruction was performed in two cases, and partial reconstruction was performed in 14 cases. Among these cases, eight were due to partial infection of the aortic valve annulus and residual cavity in the LVOT. After reconstruction of the valve annulus, a 4.0 mm hole was created on the left ventricular side. The remaining six cases, which had less severe annular involvement, underwent valve replacement directly after complete removal of the affected area. Additionally, in three cases, a biopatch was used to reconstruct the aortic-mitral fibrous continuity, because of disruption. In one case, a small aortic root (17 mm) was enlarged with a patch before mechanical valve replacement. Three patients underwent the Bentall procedure, whereas the remaining 18 patients underwent simple aortic valve replacement, including 13 mechanical valves and 8 bioprostheses.
All patients survived postoperatively with improved cardiac function, and no deaths occurred. Two cases of acute renal failure occurred postoperatively, both of which recovered after continuous renal replacement therapy. A follow-up chest radiograph 1 month after discharge showed a reduced cardiac silhouette, and echocardiography revealed a significant decrease in both left atrial and left ventricular size, with no significant change in ejection fraction. During follow-up, all patients had normal function of the aortic prosthetic valve, showing no occurrences of prosthetic valve-related IE, paravalvular leak, aortic root abscess, or third-degree atrioventricular block. The overall outcomes were favorable.
Perioperative adjustment of cardiac function is crucial. In addition to antibiotic therapy, optimizing the patient’s systemic condition within the limited preoperative window is essential. Emergency surgery should be considered for patients with uncontrollable heart failure, infection, large vegetations (≥10 mm), or severe arrhythmias [4]. For relatively stable patients, surgery should be delayed until the infection is effectively controlled, the heart failure is stabilized, and systemic symptoms improve. IE involving the aortic annulus results in periannular or root abscesses, or infected cavities at the aortic-mitral junction [3]. Current guidelines recommend complete debridement and annular reconstruction, but offer limited guidance for managing LVOT cavities [1, 5]. Leontyev et al. have evaluated the surgical outcomes in patients with active infective endocarditis complicated by aortic root abscesses, and their findings have indicated high mortality rates in these cases [3]. For patients with uncontrolled infection or those with large residual cavities at the aorto-mitral continuity caused by the infection, we recommend patch reconstruction of the LVOT with perforation (Figure 1). A residual cavity in the LVOT may lead to turbulence and blood stasis, thereby increasing the risk of infection and paravalvular leakage. Creating a perforation on the left ventricular side as close as possible to the residual cavity can decrease turbulence, promote blood flow, decrease stasis, and thus prevent abscess formation while enhancing the effectiveness of antibiotic treatment. However, improper placement or size of the perforation may impair valve reconstruction and increase the risk of postoperative complications, including paravalvular leak, thromboembolism, and heart failure. The standard approach typically involves valve replacement, and the Bentall procedure is reserved for patients with aortic valve and ascending aortic infection. Additionally, age and infection severity should be considered in choosing a valve. Bioprosthetic valves are frequently recommended because of their potent anti-infective properties and low hemodynamic impact. Valve replacement is performed by using interrupted sutures, and gaskets are typically placed on the aortic side. For newly constructed aortic annuli or after root enlargement, the gaskets are generally placed on the outer side of the aortic wall.
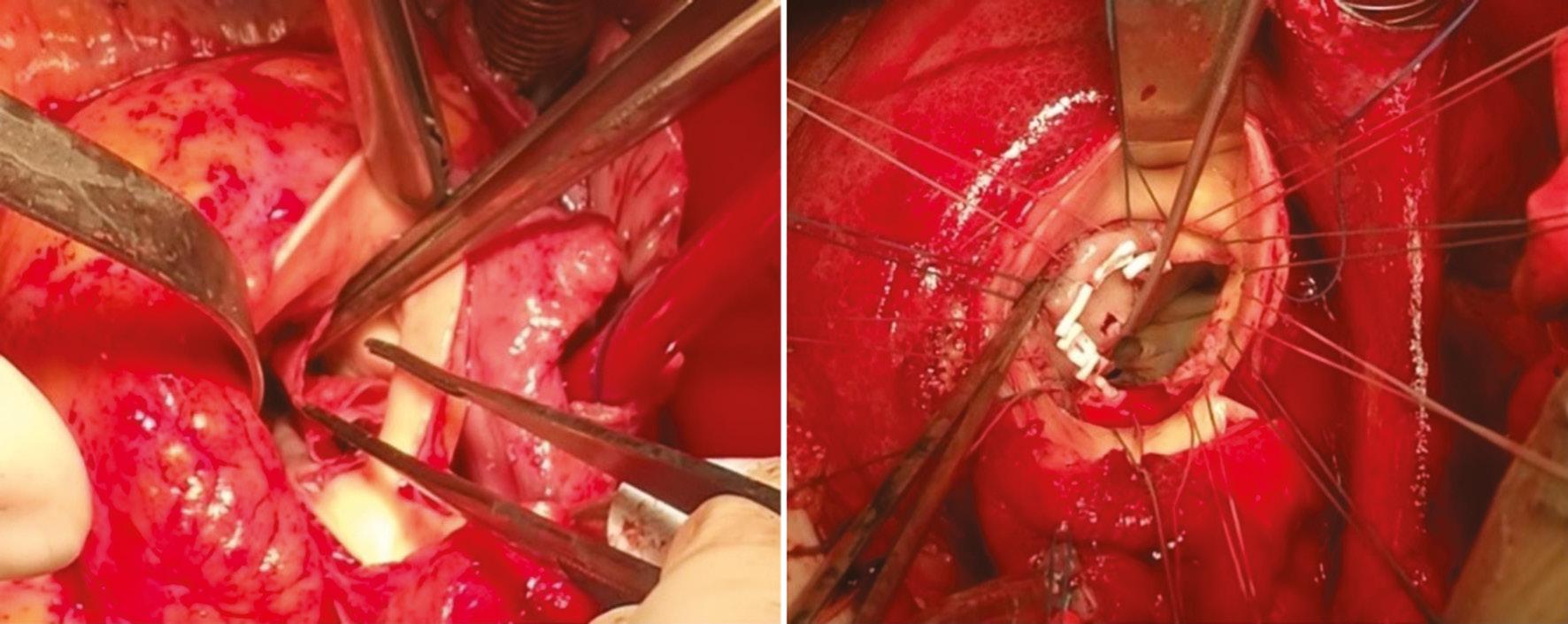
Perforation of the Left Ventricular Outflow Tract After Biopatch Reconstruction of the Aortic Annulus (4.0 mm).
IE with aortic annular involvement is a complex, life-threatening condition requiring prompt surgical intervention. Timely surgery is crucial for patients with refractory heart failure, persistent infection, large vegetations, or severe arrhythmias. The surgical approach should be tailored to each patient’s specific anatomy and pathology. In cases with a large residual cavity in the LVOT or during the acute infection phase, creating a perforation on the left ventricular side during annulus reconstruction can prevent aortic root abscess formation and enhance local antibiotic efficacy. Further large-scale, controlled studies are needed to confirm the effectiveness of the technique. Additionally, ongoing research and long-term follow-up will be essential to identify risk factors for poor outcomes, and improve surgical techniques and perioperative care, thus ultimately enhancing patient survival and quality of life.

